Abstract
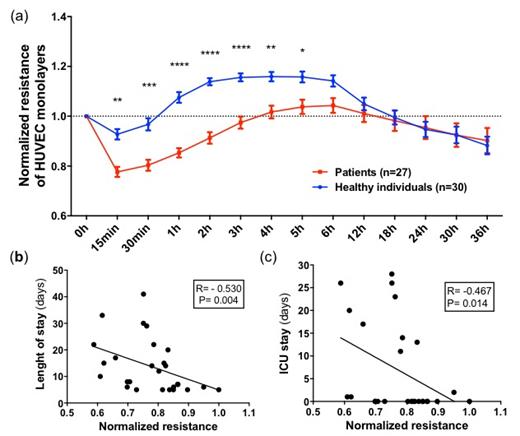
Background: the pathogenesis of severe COVID-19 involves the deregulated activation of different compartments of immunothrombosis, which are otherwise important for pathogen eradication and tissue repair. Coagulation activation, angiogenesis and alterations of endothelial barrier (EB) are elements of immunothrombosis that have been shown to be involved in the pathogenesis of COVID-19. Angiopoietins (Ang) 1 and 2 and their receptor Tie2 and VEGF-A are well-known pro-angiogenic mediators that, during inflammation also mediate EB disruption. Recently, it has also been demonstrated that the Ang/Tie2 pathway is involved in coagulation activation. Here we explored whether increased levels of angiogenesis/EB regulators (which have been previously associated with disease severity in COVID-19) are also associated with both EB disruption and coagulation activation in this condition. Methods: the study population consisted of 30 patients with COVID-19 confirmed by RT-PCR and presenting typical CT findings admitted due to hypoxemia. Thirty sex- and age-matched healthy individuals were recruited at the same time, from the same geographic region. Patients were part of a clinical trial (REBEC: U1111-1250-1843) but samples were obtained before any study intervention, within 24 hours from diagnosis confirmation. Circulating levels of angiogenesis/EB regulation mediators and coagulation biomarkers were measured by commercial assays (immunological or functional). Monolayers of endothelial cells from umbilical veins (HUVECs) or lung (HULECs) were used for measurement of EB integrity using an impedance sensor system (ECIS, Electric Cell-substrate Impedance Sensing System). Cells were stimulated with serum from patients or healthy individuals and EB integrity was continuously monitored for 36 hours. Clinical outcomes were obtained from the digital medical records. Results: mean length of hospital stay (LOS) was 12.9 ± 9.8 days. Twelve patients (40%) required intensive care (ICU) and 28/30 patients survived. Mean D-dimer was 3,609 ± 14,440 ng/mL. Circulating levels of Ang1, Ang2, sTie2 and VEGF-A were all significantly increased in patients compared to healthy individuals (Ang1: 463.2 ± 194.6 vs 237.4 ± 104.9 pg/mL, p<0.0001; Ang2: 1,926 (1,275 - 3,134) vs 1,215 (9 - 1,440 pg/mL), p<0.0001; Tie2: 10,753 ± 2,377 vs 8,603 ± 1,851 pg/mL, p<0.0001 and VEGF-A: 94.7 (73.4 - 116.0) vs 45.9 (39.7 - 57.0 pg/mL), p<0.0001.). In contrast, soluble VE-cadherin levels were decreased in patients compared to healthy individuals (1,234 ± 318 vs 1,539 ± 363 ng/mL, P=0.001). Serum from COVID-19 patients induced decreases of EB integrity in monolayers of both HUVECs and HULECs as early as 15 minutes, lasting up to 5 hours after stimulation (figure 1). The magnitude of EB disruption was correlated with clinically relevant outcomes such as time of ICU stay and LOS (figure 1). Interestingly, levels of Ang1, Ang2 and soluble VE-cadherin levels were also significantly correlated with the magnitude of EB disruption, as well as with biomarkers of coagulation activation such as fibrinogen, Von Willebrand Factor antigen levels, PAI-1, P-selectin and urokinase receptor (uPAR). Conclusions: Ang-1/Ang-2 mediated Tie2 signaling has been shown to be important for the fine regulation of barrier integrity and coagulation activation at the endothelial level, which are two critical elements of immunothrombosis. Our results provide evidence supporting that the interplay between these processes can play a role in the mechanisms driving COVID-19 severity, and suggest that targeting the Ang/Tie2 and VEGF-A pathways could be attractive strategies to modulate not only changes of the alveolar-capillary barrier, but also of coagulation activation in COVID-19.
Figure 1. In (a), endothelial barrier (EB) integrity of HUVEC monolayers upon stimulation by serum from COVID-19 patients and healthy individuals (n=27-30 per group). The lower the normalized resistance, the higher the magnitude of EB disruption. Significant differences (* to ****) are evident from 15 min to 5 hours (Anova corrected for multiple comparisons). In the lower panels, the correlation of EB disruption with clinically relevant outcomes such as length of hospital stay (b) and days of intensive care (c) are shown. Negative correlations (Spearman test) indicate that the magnitude of EB disruption is associated with worse outcomes.
No relevant conflicts of interest to declare.